Clinical Case Study: Ophthalmic Vein Thrombosis

Clinical Case Study: Ophthalmic Vein Thrombosis Presenting as Ocular Redness and Vision Loss
-David A. Reichstein, M.D.
Red eye and vision changes are common presentations in ophthalmology. While inflammation, infection, and even intraocular tumors are frequent considerations, rarer vascular conditions can mimic these more typical diagnoses. This case highlights the importance of maintaining a broad differential diagnosis when evaluating acute ocular changes.
Clinical Presentation
A patient presented with progressive vision loss, redness, and swelling of one eye. The initial diagnosis elsewhere was iridocyclitis, and the patient was treated with topical corticosteroids. However, the rapid onset of symptoms, associated headaches, and external findings of engorged conjunctival vessels and proptosis raised concern for an alternative diagnosis.
Examination and Imaging
On examination:
- Vision was moderately reduced in the affected eye.
- Conjunctival and scleral vessels were markedly dilated and tortuous.
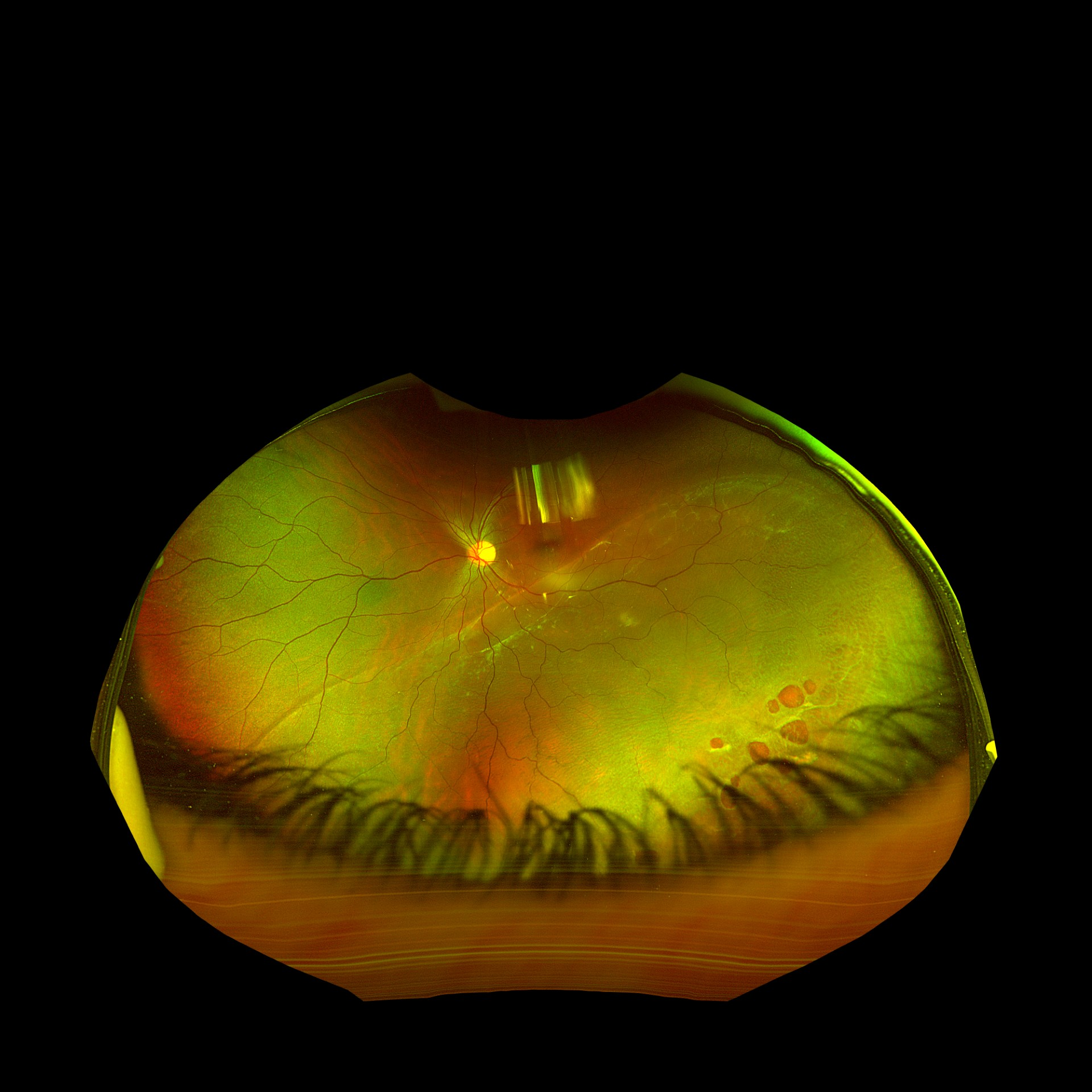
- Choroidal detachments and intraretinal hemorrhages were observed.
- Ultrasound confirmed diffuse choroidal detachments with no mass lesion.
CTA and MRI revealed thrombosis of the superior ophthalmic vein, without evidence of cavernous sinus thrombosis.
Management
The patient was promptly referred to the emergency department and started on systemic anticoagulation. Steroid drops were discontinued, and the patient was transitioned from heparin to an oral anticoagulant for long-term management.
Clinical Course
- At 1 week: vision and intraocular findings showed early improvement.
- At 2 months: near-complete resolution of hemorrhages and choroidal detachments, with significant visual recovery.
Discussion
Ophthalmic vein thrombosis is a rare but serious condition that can mimic more common ocular diseases, including uveitis or choroidal melanoma. Prompt recognition and systemic management are essential to prevent vision loss and to address the underlying systemic risk factors, such as hypertension or hypercoagulability.
This case underscores the importance of:
- Considering vascular causes when evaluating acute ocular redness and vision loss.
- Utilizing imaging (CTA, MRI/MRV) early when atypical features are present.
- Coordinating care across ophthalmology, radiology, neurology, and primary care to ensure comprehensive treatment.
Conclusion
What appeared to be a routine case of ocular inflammation was ultimately identified as ophthalmic vein thrombosis. Through prompt multidisciplinary care, the patient achieved significant visual recovery and systemic stabilization.