Understanding Proliferative Diabetic Retinopathy
Understanding Proliferative Diabetic Retinopathy (PDR): A Serious Complication of Diabetes
Diabetic retinopathy is a common complication of diabetes that affects the retina—the light-sensitive tissue at the back of the eye responsible for sharp, detailed vision. Over time, high blood sugar can damage the small blood vessels in the retina, which may lead to vision-threatening conditions. One of the most serious forms is Proliferative Diabetic Retinopathy (PDR).
What is Proliferative Diabetic Retinopathy?
PDR is an advanced stage of diabetic retinopathy. Prolonged damage to retinal blood vessels can cause poor circulation in the retina and macula, leading the eye to produce new, abnormal blood vessels in an attempt to restore blood flow.
Unfortunately, these vessels are fragile and prone to complications, including:
- Bleeding into the eye (vitreous hemorrhage), which may cause sudden vision loss or floaters.
- Scar tissue formation, which can pull on the retina and lead to retinal detachment.
- Neovascular glaucoma, where new vessels grow on the iris, clogging drainage and raising eye pressure.
Left untreated, PDR can cause severe vision loss and, in some cases, blindness.
Who is at Risk?
Anyone with diabetes—type 1 or type 2—can develop diabetic retinopathy, and certain factors increase the risk of PDR:
- Longer duration of diabetes
- Poor blood sugar control over time
- High blood pressure and high cholesterol
- Pregnancy
Certain medications, including some diabetes and glaucoma treatments, as well as medications for cancer or multiple sclerosis, may also increase the risk of complications like diabetic macular edema.
Symptoms to Watch For
PDR can develop without noticeable symptoms in the early stages. As the disease progresses, symptoms may include:
- Blurred or double vision
- Floaters or dark spots in vision
- Shadows or loss of parts of your visual field
- Eye pain or pressure
Because early PDR may be asymptomatic, regular eye exams are critical for anyone with diabetes.
Diagnosing PDR
Comprehensive dilated eye exams are the standard for detecting diabetic retinopathy. During the exam, an ophthalmologist looks for signs of:
- Swelling in the retina (diabetic macular edema)
- Poor retinal circulation (retinal ischemia)
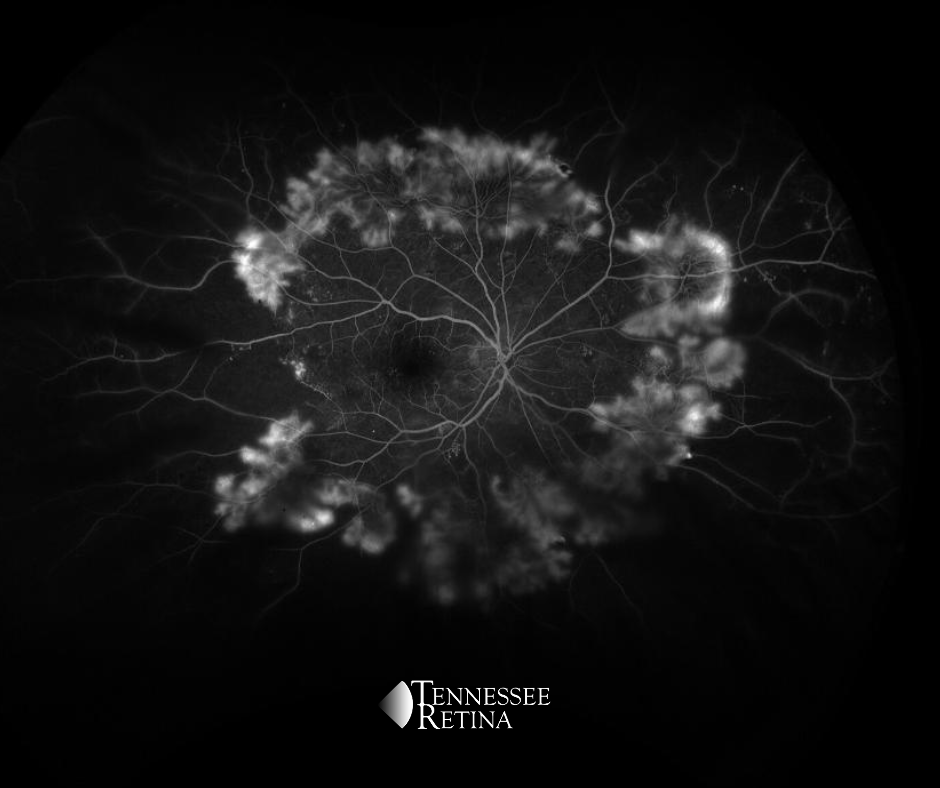
- Abnormal new blood vessel growth (neovascularization)
Additional imaging tests may include:
- Optical Coherence Tomography (OCT): Provides detailed cross-sectional images of the retina to detect fluid or swelling.
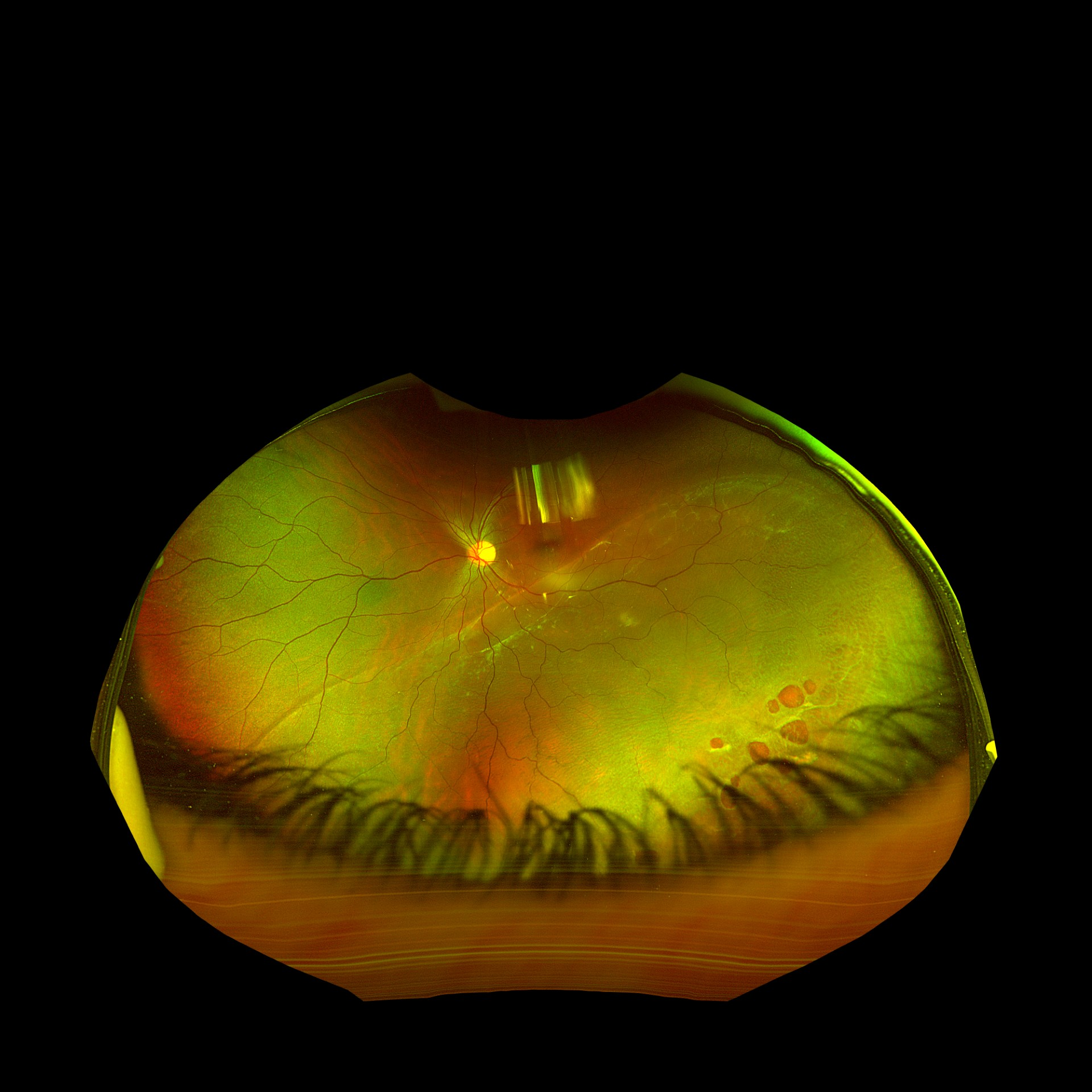
- Fundus Photography: Captures images of the retina for monitoring disease progression.
- Fluorescein Angiography (FA): Uses a special dye to visualize blood flow in the retina and detect leaks or blockages.
Treatment Options
While early diabetic retinopathy can sometimes be managed with strict blood sugar control, PDR requires prompt treatment to prevent vision loss:
- Anti-VEGF injections: Medications injected into the eye to block abnormal blood vessel growth and reduce fluid leakage.
- Laser photocoagulation: Targets abnormal vessels to prevent bleeding and further growth.
- Vitrectomy surgery: Removes blood or scar tissue in severe cases to preserve or restore vision.
Even with treatment, not all vision loss can be reversed. Retina specialists can also guide patients to rehabilitation resources and adaptive tools for living with vision impairment.
The Importance of Early Detection
Because PDR often has no early symptoms, regular dilated eye exams are essential for people with diabetes. Early detection and timely intervention significantly improve the chances of preserving vision and quality of life.